The future of equine disease research and collaboration was witnessed during the EPM Society’s Workshop in October 2017. The first workshop was held in 2014 in Kentucky, where 45 attendees gathered with the goal to better understand EPM, share information, identify unresolved areas and promote collaborative research. A similar number gathered in Tahoe City, California, October 25-27, for an intensive 1.5 days of presentations and discussion.
Another notable future that arrived was that more than half of the attendees were female, and there were infants and small children present and welcomed by the group. This is to be expected now that equine veterinarians have turned the gender curve to having nearly equal numbers of women and men practitioners. And it seems that equine research is on the same gender-equality road, with 16 of the 22 presentations being given by women and all of the younger research presenters being female. That is promising for the future of equine protozoal research.
A lot has been learned since Dr. Jim Rooney and colleagues from New Bolton Center, the University of Pennsylvania and the University of Kentucky first described what is now known as EPM. It was first called “focal myelitis- encephalitis in horses” in an article published in The Cornell Veterinarian in 1969 (which can be found at https://babel.hathitrust.org/cgi/pt?id=uc1.b3779845;view=1up;seq=518).
While EPM is a disease that was recognized nearly 50 years ago—and a lot has been learned about the causes, treatments and preventions for the disease—the group agreed that there is still much to learn. And they stated that the future of that learning process must be collaborative to a large extent.
The 2014 EPM Workshop ended with the thought that considerable progress had been made in the areas of biology, the genome and life cycle of Sarcocystis neurona ; the epidemiology and pathogenesis of EPM; the diagnosis of S. neurona and N. hughesi (which can cause EPM); and treatment.
It was also agreed in 2014 that the fields of needed research included:
• the effect of parasite genotype on pathogenesis;
• the horse as intermediate versus accidental host;
• the role of immune response in protection and disease;
• the contribution of co-morbidity (co-infection); and
• expanded fundamental knowledge on N. hughesi .
While some of these areas have been addressed by research, none has been definitively answered.
The updated EPM consensus statement released in 2016 is available to the public at http://onlinelibrary.wiley.com/doi/10.1111/jvim.13834/full.
The Future of EPM Research
Six topics for presentations and discussion at the 2017 Workshop were outlined: biology; genetics, immunology and vaccine; co-morbidity between Apicomplexan protozoa; laboratory diagnostics; future needs in the field of EPM; and treatment and prevention. The keynote talk was presented as a stand-alone on Friday morning.
One of the keynote speakers addressed an area that Nicola Pusterla, DrMedVeT, MedVet, of the University of California, Davis, College of Veterinary Medicine, said needed attention. This area is to look at “closely related pathogens and try to translate that to the pathogen we are dealing with.”
Jereon Saeij, PhD, Associate Professor and Researcher Pathology, Microbiology and Immunology, University of California, Davis, has been studying Toxoplasma gondii for the last 15 years. Saeij is new to the field of Sarcocystis and EPM research, and he said there is still a lot to be discovered about the parasites that cause EPM. He brought up some very interesting questions and observations about EPM during his presentation: “What if—a comparative approach to the Apicomplexan protozoal organisms.”
The other keynote speaker was Patricia Conrad, DVM, PhD, Professor and Researcher Pathology, Microbiology and Immunology, at the University of California, Davis. Conrad was awarded the 2017 AVMA Lifetime in Excellence Research Award. She been working on protozoal parasites for 37 years.
One of the points that Conrad raised is whether horses are really aberrant hosts in the S. neurona life cycle. It has been proven that N. hughesi can recrudesce from the latent bradyzoite state and proliferate again, and that there can be vertical transmission from a dam to a fetus. Could the same be true of S. neurona? Most research suggests this does not occur routinely.
Saeij asked the audience to ponder why some animals get sick after infection with a particular parasite strain while others do not. He posed that some individuals are more susceptible than others, and some strains of a given parasite are more virulent than others.
“Differences in disease outcome are caused by the complex interaction between host genotypes and parasite genotypes with environmental variation, which can include co-infection,” said Saeij. “Parasites have figured out how to manipulate a host to stay with it the rest of the host’s life. But how do they evade a competent immune response?”
Saeij said that Apicomplexan parasites are a leading cause of human and livestock diseases worldwide. “There are hundreds of Sarcocystis species, most have two-host life cycle (carnivore and herbivore), and some have one host. S. neurona, unlike most Sarcocystis species, can have multiple intermediate hosts.”
He noted that Sarcocystis parasites need to keep their host alive, as only the chronic encysted form is infectious—so it can’t complete its life cycle if the host dies too soon after infection.
“Parasites secrete proteins to control the immune response to form lifelong infections,” noted Saeij. “If this is a multi-host parasite, how is Sarcocystis able to evade immune responses in different species?
“Nothing is known about how S. neurona modulates the host cells it infects,” he added.
Saeij said there is a lot of “basic” knowledge that is missing in the study of S. neurona. “Mice are not a good model to study pathogenesis of S. neurona,” he noted. “S. neurona is missing ROP18 and ROP5, which are effectors secreted by Toxoplasma to inhibit host IFN-gamma- induced, immunity-related GTPases (IRGs) that are involved in killing the parasite, and therefore likely extremely susceptible to IFN-gamma mediated killing. So only IFN-gamma knockout mice can be infected by S. neurona.”
His emphasis was that this is not a “natural” state of the parasite’s life cycle and thus didn’t provide information on how S. neurona was interacting with a natural host.
“Horses, cats, opossums, skunks and humans do not have TLR11, which is the main innate immune receptor in mice that recognizes Toxoplasma and other apicomplexan parasites, and they do not have IRGs,” he noted. Therefore, these species must have other ways of recognizing and destroying parasites such as S. neurona.
“Nothing is known about how S. neurona modulates the host cells it infects,” he concluded.
It should also be noted that the natural life cycle of N. hughesi is not known.
There is no good animal model to test for differences in virulence for S. neurona strains, noted Saeij. “If we knew what virulent S. neurona strains were, and which ones were avirulent, we could cross them in possums and test virulence of the F1 progeny,” he said.
He said an alternative solution was to improve serodiagnostics so that different strains of S. neurona could be distinguished and association studies between S. neurona strains and EPM could be performed.
“S. calchasi is closely related to S. neurona and causes pigeon protozoal encephalitis,” said Saeij. “Is this a possible model for S. neurona?”
When Saeij said he did not feel that mice were a good animal model for S. neurona research, it caused a bit of debate about using mice among the researchers.
“We gave TLR11 knockout mice S. neurona and didn’t hurt them,” said Saeij. “Mice can kill S. neurona through IRGs. And the way mice deal with Sarcocystis is different from the way the horse and opossum deal with Sarcocystis, as these species do not have IRGs.”
Antoinette Marsh, JD, MS, PhD, Associate Professor, Service Head of Veterinary Medical Center Diagnostic Parasitology, Department of Veterinary Preventive Medicine, The Ohio State University, acknowledged that raccoons are difficult to work with in the lab in response to another audience member’s question on lab animal models. She said her lab has looked at ferrets.
Marsh also discussed the point that there are at least two horse strains of S. neurona that produce small cysts rather than large cysts. “We don’t have good markers to know if they are metrocytes or bradyozoites,” she said.
Saeij noted that with toxoplasmosis, when a strain is always passed through mice vs. always passed in vitro , and when these strains are then used to infect a host, the host can react differently in terms of virulence. “In vitro, the strains often become more virulent,” he said. “So how a strain has been treated in the laboratory can influence phenotypes.”
That raised discussion on where isolates used in research had been cultured, where they have traveled, and how they have been handled.
Conrad noted that some “isolates” could be a combination of different strains, or they could have had a metabolic change in the laboratory setting.
Dan Howe, PhD, a professor at the University of Kentucky’s Gluck Equine Research Center, said the idea of metrocytes (transition stage between merozoite and bradyzoite) being able to recrudesce is intriguing. “How long do metrocytes hang around?” he asked colleagues in the audience.
Marsh’s response seemed to sum up what the audience members thought: “I don’t know.”
Conrad asked whether the audience members thought strain differences among Sarcocystis species should be considered by researchers when the question is raised as to why so many horses are infected and only a small proportion get disease.
Several in the audience agreed that a “hotspot” of disease would occur if there was a more virulent strain in an area.
Conrad noted that opossums can be infected with different Sarcocystis strains. “Opossums appear to be different from cats in shedding,” she said. “Maybe opossums are persistent shedders, not onetime shedders. But what are they contaminating the environment with? You can’t even say ‘keep possums off or out of feed,’ because once opossums poop and it rains or snows, it washes in. The oocysts are in soil and wash into water supplies. They last a long time.”
Pusterla asked the audience how hard it is to genotype Sarcocystis. Conrad said that if the right laboratories had access to the parasites, it would be easy.
Resources for Veterinarians and Students
Pusterla said, “We’re all experts in our fields, but we are a small group. Each of us can make a contribution in our fields. Our colleagues are faced with the challenges out in the field. Our goal and responsibility is to come up with tools to address EPM.”
Among the topics where researchers felt they could help veterinarians in the field were helping to create guidelines for case assessment and for conducting a comprehensive neurologic exam.
“We think most vets know how to do a neurologic exam,” said Pusterla. “Sometimes there is no reason to suspect EPM.”
Pusterla added, “I’m not seeing people doing CSF taps.” Perhaps, he said, we need to show them techniques that are easier and safer when they have to sedate and test these horses.
There was discussion by Michel Levy, DVM, from the University of Calgary, about creating case simulations for veterinary students. Many in the audience thought that when the information was pulled together for these case simulations, they should also be made available to practicing veterinarians. Levy has been working with a woman in Montreal who retired from creating training for astronauts. He wants to put together virtual computer cases from history to pathology. The cases will also have different client types, from the “spend anything” to “I can’t afford to test, only treat” types.
Levy wants to create a consortium of cases for this online education. Included in the education would be different ways to do a spinal tap.
Monica Aleman, MZV, PhD, DACVIM-Internal Medicine Large Animal Internal Medicine, DACVIM-Neurology Veterinary Neurology and Neurosurgery, University of California, Davis, noted that it was important that these cases be accessible to veterinarians. “You need specialized training in neurology to see some of these things,” she explained. “I took special training, and it really opened my eyes.”
Pusterla recommended that when this online education was created, there should be a consultation portal to make it easy for veterinarians to connect with experts in the field of protozoal parasites.
The discussion turned from online education to the need for a repository of samples that researchers could use.
“We don’t have a repository of what we need,” said Pusterla. “Can we come up with group agreement for a ‘wish list’ of samples and who keeps track of them? What kind of financial support can we get to provide this?” He explained that it would be like OIE centers for equine influenza.
The audience members agreed that researchers needed “gold standard” cases for reference. “Absolutely,” said Pusterla. “We would have to have a questionnaire to have specific information and samples.”
Conrad said that the repository would need to identify the pathologists who are interested in protozoa and let them work out some of the logistics, such as how samples are shared and who pays for the personnel and facilities needed.
“We would need restrictions as to client information and the ability to use samples for other purposes,” she noted. “And we would need a collaborative team that includes pathologists.”
Pusterla reminded the audience that something of this nature would need to start with the clinicians. “We need a well-documented case that makes it to pathology,” he noted. “We need a good history, and they need to be terminal cases that then go to pathology. Perhaps we start with referral hospitals.”
Sharon Witonsky, DVM, PhD, DACVIM, Associate Professor Equine Field Service, Department of Large Animal Clinical Sciences, Virginia-Maryland College of Veterinary Medicine, said the group would need to get people together to determine key questions of case definition and have everyone possible collecting samples. “When it takes 2.5 hours to sample a brain and spinal cord, we need to share for collaborative purposes and authorship,” she said.
Levy added that the reference information should include some difficult or different cases as differential diagnoses.
David Wilson, BVMS, MS, Professor Emeritus Medicine & Epidemiology, University of California, Davis, College of Veterinary Medicine, said the group would also need “gold standard” negative cases. That elicited discussion as to whether those negative cases should be from areas without S. neurona (Europe, for example) or should be negative horses from areas where EPM is known to occur.
Conrad added, “We need to use animals that underwent all the same diagnostics and pathologic sampling. We need to come to consensus on that.”
Following are short synopses of several of the presentations at the 2017 EPM Society Workshop.
Size Matters
Marsh and colleagues recently completed a study where they found small sarcocysts that probably were missed in previous studies. “Our results also highlight the importance of immunohistochemistry staining for detecting the small sarcocysts that can be missed due to their size and lack of associated inflammation,” she reported.
During the question-and-answer session, an audience member noted that a Michigan paper stated that horses are capable of having cysts in the tongue.
Seroprevalence of S. neurona and N. hughesi Among Healthy U.S. Horses
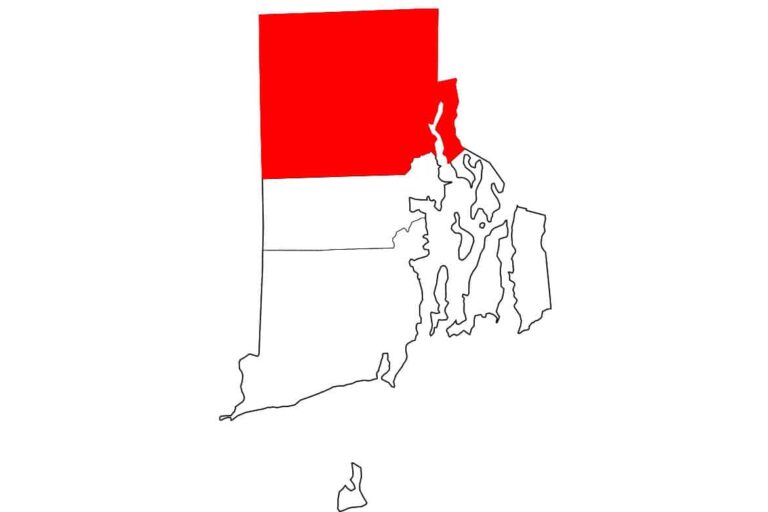
Kaitlyn James, PhD, a research assistant in the College of Veterinary Medicine at the University of California, Davis, did a study to describe the general seroprevalence of S. neurona and N. hughesi. She also looked at the potential risk factors (geographic region, breed, use, gender and age) of the horses involved in the study.
A total of 5,250 samples from 18 states was collected with risk factor information. The overall prevalence of S. neurona was 78%, while the overall prevalence of N. hughesi was 34%. Thirty-one percent were seropositive for both parasites, and 18% were seronegative to both.
S. fayeri Infection Associated with Neuromuscular Disease in Horses
Two years ago, Aleman and colleagues published an article about equine infections with Sarcocystis species. She referenced a Japanese study showing that humans who consumed raw horse meat had a S. fayeri-induced toxicity that caused intestinal sarcocystosis.
Aleman and colleagues found that S. fayeri infection was common in young, mature equids with neuromuscular disease. “Our study did not establish causality, but a possible association (8.9% of cases) with neuromuscular disease; the assumption of S. fayeri sarcocysts in muscle being an incidental finding in every case might be inaccurate. Further studies are needed to determine the role of S. fayeri infection in the development of neuromuscular disease in horses.”
Questions from the audience centered around which parasite is actually causing disease when both S. neurona and S. fayeri are a co-infection in the same horse.
One audience member said it might be possible that when S. fayeri releases toxin, it might cause neurologic disease, compared to S. fayeri that doesn’t release toxin.
Proportional Morbidity Rate of EPM in North America
Frank Andrews, DVM, DACVIM, of the Louisiana State University Veterinary Teaching Hospital, had a two-fold reason for this study. The first reason was to assess temporal changes in the proportion of cases reported to vet teaching hospitals in North America. The second was to assess the perception of veterinary practitioners regarding the incidence (cases seen) of EPM.
This was a retrospective study 1990- 2015 of case records from Veterinary Teaching Hospitals in North America and a survey sent to veterinarians via several major veterinary Listservs in 2016.
Andrews reported on the proportional morbidity rate (PMR), which is the number of cases of a specific diagnosis divided by the total number of cases of all diagnoses in that same population. He noted that a PMR is an indicator of incidence in veterinary teaching hospitals, but not of actual incidence in the whole horse population at large.
The spike in cases seen from 1995 to 1999 was probably due to the introduction of the Western blot test to diagnose EPM, after which more cases were recognized. With this exception, the PMR from veterinary teaching hospitals (1990-2008) showed little change and was approximately 0.80 (8 EPM cases/1,000 cases presented).
“However, for the past seven years (2009-2015) of the study, the number of EPM cases presented to veterinary teaching hospitals has significantly decreased,” noted Andrews. This might indicate that more practitioners are diagnosing and treating horses with EPM in their practices and not sending them to veterinary teaching hospitals, because veterinarians’ perceptions, during that time, showed that a majority thought the number of cases was staying the same or increasing.
“It appears that Standardbreds, Tennessee Walking Horses, Thoroughbreds, warmbloods, stallions and horses 3-7 years of age and 11-15 years of age are more likely to be diagnosed with EPM,” noted Andrews.
He said it is important for horse owners to consult with their veterinarians so that other causes of neurologic disease can be ruled out. However, with improved diagnostics and three available treatment options, practitioners are likely treating more EPM cases in the field and referring fewer cases to veterinary teaching hospitals.
Vaccination Development
While there was a lot of discussion about this topic, the consensus was that there is no viable vaccine at this time that has been proven to protect horses from the causative parasite. More research is needed.
Co-Morbidity Between Apicomplexan Protozoa
Martin Furr, DVM, PhD, DACVIM, is the head of the Department of Physiological Sciences at Oklahoma State University’s Center for Veterinary Health Sciences. He and Conrad co-authored a presentation on co-morbidity between apicomplexan protozoa, with Furr making the presentation.
Furr said that survival and growth of infectious protozoa in immunocompetent hosts meant that the parasites had “outrun” the host response by fast replication or mutation. It also meant that they impair development of expression of immunity in the host (immune evasion or restriction).
“The result is a ‘non-sterilizing’ immunity, which reduces parasite burden and limits pathological damage without wiping out the invader,” stated Furr.
Protozoan co-infections (polyparasitism) is common in humans, noted Furr, who said that might be the norm rather than the exception with protozoa. He said there are known co-infections in cats. In a 2014 study from Pusterla, where he looked for co-infections with S. neurona and N. hughesi in 3,123 EPM suspect horses, the researchers found that 71% of the horses were negative to both parasites; 26.8% were positive only for S. neurona; 1.2% were positive for N. hughesi only; and 0.8% were positive for both parasites.
The questions raised by the researchers included:
• Does Sarcocystis infection caused immunosuppression, allowing secondary infections with other organisms?
• To what degree does this immunosuppression limit treatment efficacy?
• Are other parasitic, bacterial or viral co-morbidities influencing EPM susceptibility?
• Do infections with various strains of S. neurona or N. hughesi influence disease susceptibility or clearance of organisms?
Laboratory Diagnostics
The overview of laboratory diagnostics for EPM was presented by Jennifer Morrow, PhD, of Equine Diagnostic Solutions, and Amy Johnson, DVM, Assistant Professor of Large Animal Medicine and Neurology, University of Pennsylvania, New Bolton Center.
The 2016 ACVIM Consensus Statement noted that there are three recommendations for the diagnosis of EPM:
1. a neurologic exam to confirm clinical signs;
2. the exclusion of other potential diseases; and
3. immunodiagnostic testing of serum and CSF to confirm intrathecal antibody production.
Johnson and Morrow presented tables of comparisons that were modified from the 2016 ACVIM consensus statement that looked at
• commercially available immunologic tests for antibodies against S. neurona;
• commercially available immunologic tests for antibodies against N. hughesi; and
• test comparisons focusing on EPM caused by S. neurona.
Their summary was that serum tests are less accurate, and that the SAG2, 4/3 ratio was the most accurate compared to Western blot, SAG1 and IFAT.
Other presentations in the laboratory section included c-reactive protein and serum amyloid A (SAA) as a biomarker for EPM diagnosis; comparison of specific antibody index and Goldmann-Witmer coefficient to evaluate intrathecal immunoglobulin G production in EPM; phosphorylated neurofilament H as a potential diagnostic marker for neurological disorders in horses; and performance assessment of different diagnostic assays to identify EPM-affected horses in a clinical setting.
Relevance and Future Needs in the Field of EPM
Pusterla gave an overview of this section. For the clinician, he said there is a need for a reliably validated and potentially improved diagnostic for EPM, as well as ways to support a diagnosis without performing a CSF tap.
He said that the industry wants additional effective drugs. He noted that case definition and quantitative serodiagnostics could potentially improve the efficacy of approved drugs. To do this, he said there is a need to establish a cost-effective and reliable animal model.
Pusterla said that in the area of prevention, the industry would like a vaccine that is proven with post-licensing studies as well as better understanding of relapse/recurrence rates.
Standing Cervical Spinal Tap
Many practitioners in the field are not comfortable doing a spinal tip for EPM testing.
Pilar Camacho-Luna, an equine medicine resident at Louisiana State University School of Veterinary Medicine, working with Andrews and another colleague, described an alternative to standing lumbosacral CSF tap for EPM diagnosis.
Traditionally, the approach for a CSF tap in horses is either alanto-occipital or lumbo-sacral. The cervical approach offered less blood contamination than samples taken from the lumbo-sacral space, and Camacho-Luna said that the location was less difficult to access. The procedure was done using ultrasound- guided needle insertion.
She reminded the audience that there is always a risk associated with anesthetizing a horse that is already neurologic.
Treatment and Prevention
The final segment of the EPM Workshop started with an overview presented by Steve Reed, DVM, DACVIM, of Rood and Riddle Equine Hospital, and Rob MacKay, BVSc, PhD, DACVIM, a professor at University of Florida College of Veterinary Medicine.
The presenters noted that there have been several drugs used to treat EPM in the last 40 years. Currently there are FDA-approved therapies that include Marquis (ponazuril), Protazil (diclazuril), sulfa/pyrimethamine and a combination treatment. They noted there also are unofficial/off-label/illegal EPM treatments that include toltrazuril (Baycox) and compounded drugs.
Some immunostimulants are being used in horses with EPM. Other prevention methods include reduction of risk factors (such as stress and transportation), reduction of exposure to or contamination by opossums, and prophylactic treatment.
Reed noted that there is “promiscuous” use of EPM drugs in racehorses.
Howe reported that bumped kinase inhibitors (BKIs) might be good candidates for treatment of EPM. Pusterla discussed a positive initial study of twice-weekly diclazuril administration rather than daily administration to reduce infection rates.
There also was a long discussion about “relapses” of EPM with no clear-cut answers.
One interesting presentation was on a paper by Heather Fritz, DVM, PhD, of UC Davis diagnostic lab, and colleagues from Davis and Washington State University, entitled: “Novel high-throughput screen of drug compound library identifies inhibitors of SN growth.”
Her group developed, validated, then implemented the use of novel high-throughput screen to test 725 FDA-approved chemical compounds from the National Institutes of Health clinical collections library.
“Our screen identified 18 novel compounds with confirmed inhibitory activity against S. neurona growth,” she reported. “Many of the inhibitory compounds identified have well-defined mechanisms of action, making them useful tools to study parasite biology in addition to being potential therapeutic agents.”
They found that 15 of the 18 compounds had activity against one or more related apicomplexans.
“Interestingly, nearly half of the inhibitory compounds were reported to have activity against dopamine receptors,” she reported. “These studies demonstrate the use of a robust new tool for discovering new chemotherapeutic agents for EPM and potentially provide new reagents to elucidate biologic pathways required for successful S. neurona infection.”
Take-Home Message
The 2017 EPM Society Workshop might have been small in size, but the information should give hope to clinicians and horse owners that solving the problem of EPM is moving forward at a rapid rate. There is still much to learn, but with cooperation and a little more time, this disease can be mastered.