Herpes is a household name. It is common knowledge that once you have a cold sore, the Herpes simplex virus can recrudesce throughout your life to cause further bothersome and infectious sores.
The ability of viruses of the herpes family to “hide in plain sight” in the body is one of their more remarkable host adaptations. With host adaptation, parasites co-evolve with their natural host species to create a balance between virulence and transmissibility.
The more notorious members of the equine herpesvirus family are those that cause outbreaks of severe respiratory disease and neurological disease—equine herpesvirus type 1 (EHV-1) and equine herpesvirus type 4 (EHV-4). These viruses can be virulent in the host and are highly transmissible in respiratory secretions from infected horses.
Thankfully, vaccination, ever-more-sophisticated testing methods and increased industry awareness have helped to curb outbreaks.
Equine herpesvirus type 2 (EHV-2) and equine herpesvirus type 5 (EHV- 5) are highly host adapted, as well as ubiquitous, and until recently were considered benign after the initial infection and related mild respiratory disease.1
However, continued diligent research and more sophisticated testing methods have challenged that dogma. Equine herpesvirus type 5 has come under intense scrutiny regarding its relationship to mature horses suffering from a disease now recognized as equine multinodular pulmonary fibrosis or EMPF.2
Recently, one of Koch’s postulates (criteria to establish causative relationships between agent and disease) has been fulfilled, whereby horses experimentally infected with EHV-5 developed lung fibrosis.3 Since that time, it has been hypothesized that interactions between the host, the strain(s) of EHV-5 harbored and possibly co-infections with EHV-2 strains play a role in the ultimate development of EMPF as a clinical entity.4-6 However, although progress has been made, because both EHV-2 and EHV-5 are found in healthy equids worldwide, a diagnostic challenge is afoot.
EMPF is not a commonly diagnosed disease. Horses diagnosed tend to be mature (average age 14 years) with no gender predilection. EMPF can manifest with signs similar to several different lung diseases, including primary bacterial infection or as an infection secondary to underlying inflammatory airway disease (IAD).
Clinical signs include a combination of weight loss, decreased appetite, low-grade fever, cough, increased respiratory rate and effort, and exercise intolerance with varying degrees of respiratory distress. Usual diagnostic techniques are of little help. Auscultation of the thorax and blood work will do little to help with diagnosis. Ultrasonography of horses with EMPF will generate images of either a diffuse nodular pattern or larger demarcated areas of hyperechoic tissue, consistent with fibrosis. However, this is not pathognomonic for EMPF.
The “gold standards” for diagnosing EMPF are a lung biopsy and lung radiographs.7 While radiographs carry little risk to the horse, having the equipment to perform good thoracic radiographic studies has typically been the domain of large practices and veterinary schools. Lung biopsy carries a real and undesirable risk of hemorrhage even in the most experienced hands, making it an uninviting diagnostic tool. Tracheal wash or broncho-alveolar lavage (BAL) can be a challenge in a horse with respiratory distress, and as such, the horse that presents with low-grade fever and respiratory distress might be treated for IAD and/or bacterial pneumonia. Only when the horse does not respond to therapy might we pursue more diagnostic tests.
Recent work has shown that performing quantitative PCR (qPCR) for EHV-5 on BAL fluid or paired whole blood and nasal secretions can be supportive of a clinical diagnosis of EMPF.7 However, at this point, quality thoracic radiographs or a lung biopsy can be more readily justified to confirm a diagnosis of EMPF.
Current literature on EMPF makes for sober reading, as many horses were diagnosed on the necropsy floor or did not respond to therapy. However, the recent publication of a case diagnosed with EMPF treated with the antiviral drug valacyclovir suggests that when caught early, this disease might be curable.8 Consequently, adjusting our diagnostic testing algorithm for horses with respiratory disease to include testing for EHV-5 on appropriate samples might be our best chance for EMPF to truly become a curable disease.
Strangles
Strangles is the most-diagnosed infectious disease in horses worldwide.9 Brief mentions in ancient literature allude to the disease; Ruffus in 1251 was the first to record the clinical signs of the disease, noting pyrexia followed by abscessation of lymph nodes of the head and neck. Such easily recognized clinical signs beg the question as to why strangles continues to be a scourge of horses globally today. The answer to this question might be the biological complexity and complicated practicality of eradication.
Strangles is a highly infectious and contagious disease caused by the bacterium Streptococcus equi subspecies equi (S. equi), so named for its ability to cause swelling of the lymph nodes of the head and neck that can occlude the upper respiratory tract. S. equi is the consummately host-adapted equid pathogen.10 Genomic sequencing from outbreaks around the globe has changed the previously held notion of a stable genome and added further knowledge regarding the elegance of this organism’s host adaptation.11,12
Following infection with S. equi from contaminated water, or contact with infected material or equipment, the bacteria cross the oral and nasal mucus membranes to infect the regional lymph nodes.13 Presence of the bacteria on mucus membranes can be minimal in as little as three hours after inoculation—a feature that can lead to false negative results when testing these surfaces.14
Once in the lymph nodes, the bacteria are resistant to phagocytosis, causing abscessation and eventual rupture.15
Up to 10% of infected horses develop carrier status, with bacteria being harbored in the guttural pouch. Despite this colonization, these horses appear to be healthy.10 Carriers are key to the global success of this organism, as they can intermittently shed the organism.
Another key survival tool investigators are beginning to unravel through genomic sequencing is the ability of S. equi to survive in two contrasting environments: the guttural pouch and the lymph node. Gene loss and gene gain have been found through genome sequencing and might be relevant to diagnostic testing, as well as to the host’s immune response.
For example, differences in the unique S. equi gene, SeM , have been identified in strains harbored in guttural pouch samples vs. lymph node sample.12,16
Further complicating diagnostic testing is the enormous overlap between the genome sequences of S. equi and the ubiquitous Streptococcus equi subspecies zooepidemicus (S. zooepidemicus), which share a massive 97% of their DNA identity.11
Bacterial culture used to be the gold standard for diagnostic testing wait 48 hours for growth and the up to 56% false negative detection rate, this technique has been surpassed by DNA-based techniques. New genomic data have led to more sensitive, specific and rapid methods of detection by PCR using the traditional SeM , as well as gene targets such as seeI, eqbE 17 and SEQ2190.11
Although the biological complexity of the disease is fascinating, what are the practical implications?
In clinical practice, the questions include what to test and when. Aspirates from swollen lymph nodes are an obvious choice, but when faced with new horses entering the herd, patience, tenacity and the dedication of some financial resources are required. These practical considerations are often overlooked or under-financed and can lead to industry outbreaks of devastating magnitude.
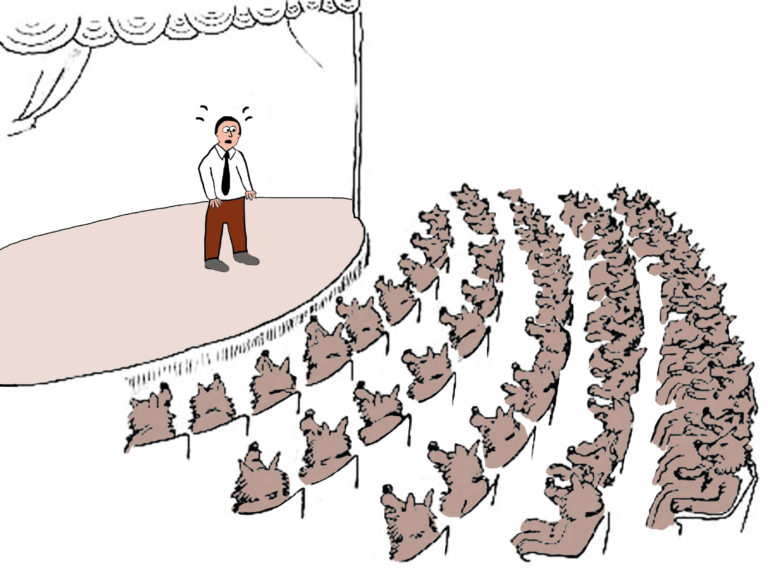
Compliance for quarantine and the testing of new horses entering a facility is the stuff of nightmares. The confusion as to what samples to procure and the challenge of maintaining dedicated staff or providing appropriate barrier clothing should not be underestimated.
Absolute consensus does not exist as to which samples are the best to submit for testing. However, most believe the current gold standard to be a one-time guttural pouch wash for laboratory PCR testing.18,19 Importantly, this sample must include wash fluid from both left and right guttural pouches, and the endoscope must be appropriately cleaned between horses. The cumbersome nature of this test might make the technique of three nasopharyngeal washes performed at weekly intervals sound like an acceptable alternative.
However, be warned: The longer period of sampling and the possibility of a false negative test result with the nasopharyngeal technique easily make the nuisance factor and expense of guttural pouch endoscopy well worth the effort.
In conclusion, while there are some new methods for diagnosing S. equi infection, the basic tenants of diligent quarantine practices, biosecurity measures and appropriate screening sample testing remain the bedrock of controlling the miserable and costly disease we call strangles.
Take-Home Message
Ongoing research on “old” diseases and agents, such as strangles and herpesviruses, can help veterinarians better understand the health problems that can be caused in horses and how those problems can be avoided. That understanding can also help you educate your clients on better management of their horses to prevent problems with diseases such as herpes and strangles.
References
1. Hartley, C.A.; Dynon, K.J.; Mekuria, Z.H.; El-Hage, C.M.; Holloway, S.A.; Gilkerson, J.R. Equine gammaherpesviruses: Perfect parasites? Veterinary Microbiology 2013;167: 86–92.
2. Williams, K.J.; Maes, R.; Del Piero, F.; Lim Wise, A.; Bolin, D.C.; Caswell, J.; Jackson, C.; Robinson, C.N.E.; Derksen, F.; Scott, M.A.; Uhal, B.D.; Li, X.; Youssef, S.A.; Bolin, S.R. Equine Multinodular Pulmonary Fibrosis: A Newly Recognized Herpesvirus-Associated Fibrotic Lung Disease. Veterinary Pathology 2007;44:849–862.
3. Williams, K.J.; Robinson, N.E.; Lim, A.; Brandenberger, C.; Maes, R., et al. Experimental Induction of Pulmonary Fibrosis in Horses with the Gammaherpesvirus Equine Herpesvirus 5. PLoS ONE 2013;8(10): e77754. Doi:10.1371/journal.pone.0077754.
4. Hue, E.S.; Fortier, G.D.; Fortier, C.I.; Leon, A.M.; Richard, E.A.; Legrand, L.J.; Pronost, S.L. Detection and quantitation of equid gammaherpesviruses (EHV-2, EHV-5) in nasal swabs using an accredited standardized quantitative PCR method. Journal of Virology Methods. 2014;198:18-25. doi: 10.1016/j.jviromet.2013.12.008. Epub 2013 Dec 24.
5. Back, H.; Ullman, K.; Treiberg Berndtsson, L.; ,Riihimäkib, M.; Penell, J.; Ståhld, K.; Valarchera, J-F.; Pringle, J. Viral load of equine herpesviruses 2 and 5 in nasal swabs of actively racing Standardbred trotters: Temporal relationship of shedding to clinical findings and poor performance. Veterinary Microbiology 2015;179: 142–148.
6. Back, H.; Ullman, K.; Leijon, M.; Soderlund, R.; Penell, J.; Stahl, K.; Pringle, J.; Valarcher, J-F. Genetic variation and dynamics of infections of equid herpesvirus 5 in individual horses. Journal of General Virology. 2016;97: 169–178 DOI 10.1099/jgv.0.000332
7. Pusterla, N.; Magdesian, K.G.; Mapes, S.M.; Zavodovskaya, R.; Kass. P/H. Assessment of quantitative polymerase chain reaction for equine herpesvirus-5 in blood, nasal secretions and bronchoalveolar lavage fluid for the laboratory diagnosis of equine multinodular pulmonary fibrosis. Equine Veterinary Journal 2017;49: 34–38. DOI: 10.1111/evj.12545
8. Schwarz, B.; Schwendenwein, I.; van den Hoven, R. Successful outcome in a case of equine multinodular pulmonary fibrosis (EMPF) treated with valacyclovir. Equine Veterinary Education 2013; 25 (8): 389-392 doi: 10.1111/j.2042-3292.2012.00425.
9. Timoney, J.F.; Strangles. Veterinary Clinics of North America; Equine Practice 1993;9, 365–374.
10. Waller, A.S. New perspectives for the diagnosis, control, treatment, and prevention of strangles in horses. Veterinary Clinics of North America; Equine Practice. 2014;30:591-607.
11. Holden, M.T.G.; Heather, Z.; Paillot, R.; Steward, K.F.; Webb, K.; Ainslie, F.; et al. (2009) Genomic Evidence for the Evolution of Streptococcus equi: Host Restriction, Increased Virulence, and Genetic Exchange with Human Pathogens. PLoS Pathog 2009;5(3): e1000346. https://doi.org/10.1371/journal.ppat.1000346.
12. Harris, S.R.; Robinson, C.; Steward, K.F.; et al. Genome specialization and decay of the strangles pathogen, Streptococcus equi is driven by persistent infection. Genome Research 2015;25:1360-71.
13. Weese, J.S.; Jarlot, C.; Morley, P.S. Survival of Streptococcus equi on surfaces in an outdoor environment. Can Vet J. 2009;50:968-970.
14. Timoney, J.F.; Kumar,P. Early pathogenesis of equine Streptococcus equi infection (strangles) Equine Veterinary Journal. 2008;40:637-642.
15. Timoney, J.F.; Suther, P.; Velineni, S.; Artiushin, C. The antiphagocytic activity of SeM of Streptococcus equi requires capsule. Journal of Equine Science. 2014;25:53-56.
16. Kelly, C.; Bugg, M.; Robinson, C.; et al. Sequence variation of the SeM gene of Streptococcus equi allows discrimination of the source of strangles outbreaks. Journal of Clinical Microbiology. 2006;44:480-486.
17. Heather, Z.; Holden, M.T.; Steward, K.F.; et al. A novel streptococcal integrative conjugative element involved in iron acquisition. Mol Microbiol 2008;70:1274-92.
18. Newton, J.R.; Verheyen, K.; Talbot, N.C.; et al. Control of strangles outbreaks by isolation of guttural pouch carriers identified using PCR and culture of Streptococcus equi. Equine Veterinary Journal. 2000;32:515-526.
19. Boyle, A.G.; Rankin, S.C.; Duffee, L.; et al. S. equi detection PCR assay for equine nasopharyngeal and guttural pouch wash samples. Journal of Veterinary Internal Medicine. 2016;30:276-281.