Of all the endocrine disorders affecting horses, equine metabolic syndrome (EMS) is the newest. This at least partly explains why so many questions persist regarding diagnosis and management. Not only do equine practitioners need to continually educate themselves regarding equine metabolic syndrome guidelines, but we also need to effectively relay the newest information to our clients.
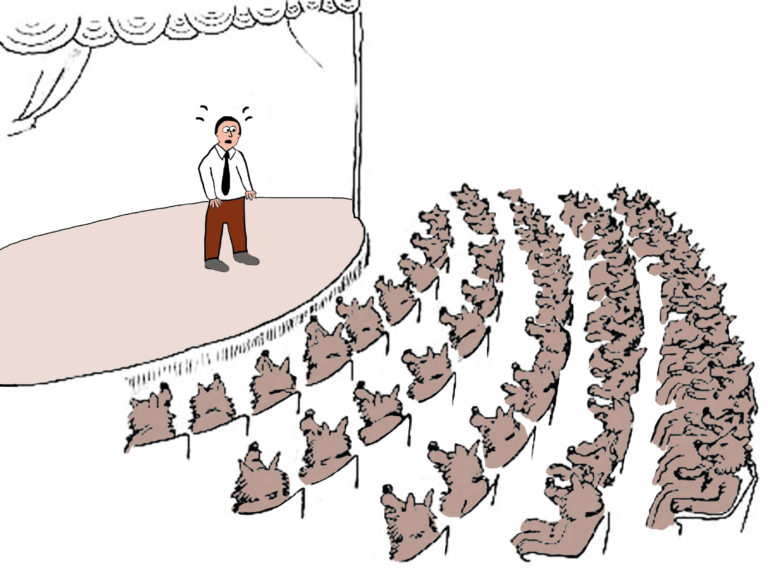
According to a recently published survey, this is no small feat (Golding et al. 2021). The survey highlighted that horse owners find equine metabolic syndrome confusing. As a result, they leave many horses undiagnosed, untreated and at risk of laminitis.
That study surveyed 491 horse owners regarding their knowledge of eight different conditions, including equine metabolic syndrome. Owners reported they had very poor knowledge of equine metabolic syndrome. One in five reported never having heard of this condition at all. That dearth of knowledge was not due to lack of experience in the equine industry. Most survey respondents (77%) were experienced or very experienced. Instead, lack of education and educational materials appeared to be a common barrier.
More than one-third of survey respondents indicated that they had not even searched for information on equine metabolic syndrome. At the same time, 43% thought that there was inadequate information available on the condition.
These data highlight the importance of client education by veterinarians. In turn, equine practitioners must also be up to date on the latest information pertaining to this disease. This article outlines the key features of equine metabolic syndrome, a brief description of the nuances associated with testing/diagnosing this condition, and the basics of managing affected horses.
The information relayed here relies heavily on the information included in the most recent guidelines on EMS published in 2019. They are available in an open access article (from Durham et al. 2019) as well as those produced by the Equine Endocrinology Group available at sites.tufts.edu/equineendogroup/.
EMS Basics
“EMS is a collection of risk factors for laminitis,” explained Nicholas Frank, DVM, PhD, DACVIM, a professor of large animal internal medicine and associate dean for academic affairs at the Cummings School of Veterinary Medicine at Tufts University in North Grafton, Massachusetts. “Insulin dysregulation (ID) is the most important risk factor. It must be present for us to say that a horse has EMS.”
According to Frank, additional factors include:
- readily becoming obese (affected horses are “easy keepers”);
- abnormal fat deposition within the neck crest, around the tail head, sheath or mammary gland, or increased internal fat stores; and
- higher than normal blood triglyceride concentrations.
Further, concentrations of hormones secreted from fat tissues (adipokines) are also affected in some horses with EMS.
“Hyperinsulinemia-associated laminitis (HAL) is the most important clinical consequence of EMS. It can lead to chronic pain and significant damage to the feet,” Frank explained.
Insulin dysregulation is defined by the presence of hyperinsulinemia and/or insulin resistance, which is a decreased ability of insulin to move glucose into tissues.
To clarify the different definitions, Frank said, “You can say that a horse has ID alone if it is the only abnormality detected or that they have EMS if any of the other risk factors are also present. In either case, ID increases the risk for laminitis. We need to lower blood insulin concentrations as soon as possible.”
The Clinical Picture of EMS

The prevalence of equine metabolic syndrome is about 20% in the general light-horse population in the United States. This condition occurs more commonly in certain horse breeds, as well as ponies and donkeys. Those might include Andalusians, Arabians, Morgan horses, Paso Finos, Shetland ponies and Welsh ponies.
Frank said that owners of horses from higher-risk breeds should be particularly concerned about equine metabolic syndrome. But, he said that all horse owners need to be aware of the risk factors for laminitis. “If a horse has a higher-than-normal blood insulin concentration, readily becomes obese or develops excess fat deposits in the neck or elsewhere on the body, then allowing them to eat high-sugar feeds or pasture grass might precipitate an episode of laminitis,” he said.
Clinical findings suggestive of equine metabolic syndrome include unexplained mild lameness (subclinical laminitis), the presence of divergent hoof rings or “founder lines” on the feet, being an easy keeper, or having a cresty neck or increased fat deposits around the tail head, sheath or mammary gland.
Be aware, however, that while obesity and a sedentary lifestyle often cause equine metabolic syndrome, not all horses with the condition are obese, and they are easier to miss. Practitioners should measure blood insulin concentrations to assess any horse that they have concerns about.
Diagnostic Testing
Practitioners can check blood insulin concentrations using two approaches. “A simple approach is to collect a blood sample after the horse has only been eating hay (no grain) and measure plasma insulin concentrations,” said Frank. “If the insulin concentration is higher than normal, the horse suffers from hyperinsulinemia and therefore ID.
“If a horse is moderately or severely affected by ID, this test will be positive. But mildly affected horses can have normal results, so the test has limitations,” Frank warned.
Cutoff values are usually provided by the referral laboratory, and the Equine Endocrinology Group recommendations are available online.
The second approach is to perform an oral sugar test (OST). This fully assesses the horse and detects mild, moderate or severe insulin deficiency. This test involves administering a measured dose of Karo Lite corn syrup to the horse by mouth and drawing blood samples 60 and 90 minutes later. Giving corn syrup stimulates insulin release, and horses with insulin deficiency have higher-than-normal responses to oral sugars.

Key Management Strategies for EMS
Generally speaking, horses with EMS are obese and sedentary, although as mentioned earlier there are exceptions to this rule. The three main ways to manage horses with EMS are:
- decrease nonstructural carbohydrate (NSC) intake;
- encourage body fat loss; and
- exercise.
There are detailed instructions on each of these three prongs of management in the 2019 European College of Equine Internal Medicine (ECEIM) EMS Guidelines. (The open access article is available at https://pubmed.ncbi.nlm.nih.gov/30724412/.) Some additional thoughts to ponder when instituting those recommendations include being sure to balance concerns about gastrointestinal health and the horse’s well-being when decreasing the amount of feed provided.
Frank noted, “Horses are designed to graze throughout the day (about 16 hours on their own devices). The grass or hay entering the stomach buffers the acid secreted and decreases the risk of gastric ulcers forming. In addition, forage quantity and quality will also impact the overall health of the intestinal microbiome, which is essential for the overall health and well-being of any horse. Housing the horse in a small paddock with a companion enhances well-being. You should also select hay with lower energy content so that larger amounts can be fed.
EMS Feeding Guidelines
The guidelines recommended:
- Consider soaking the hay (from 30 minutes to 1 hour in cold water) to lower the NSC content. But be cautious about over-soaking because it can leach important vitamins and minerals from the hay. A low-NSC ration balancer is ideal.
- Add a vitamin E supplement for EMS horses with limited access to grazing.
- For horses with moderate or severe insulin dysregulation, analyze the hay to determine the NSC content.
Testing Hay
Carey Williams, PhD, equine extension specialist and associate director of the Rutgers University Equine Science Center, described how to have hay tested. She said, “The proper and most accurate way of testing hay is using a core sampler. Some county extension offices will loan/rent these tools out. Take about three core samples from 10% of the hay in the load or batch. If that is not practical, hand grab about three samples from the center of the bale, sampling about 10% of your load of hay. Aim for at least 10 bales in a large load.”
Next, Williams advised putting the samples in a bucket and mixing them together. Transfer a subsample from the bucket into a large Ziploc bag, making sure to also get the fines, which are the small particles in the bottom of the bucket. Send that bag to an analytical laboratory such as Equi-Analytical Labs (which is the most common forage-testing facility) or a comparable company. According to Williams, there are various testing packages to choose from. Some are as cheap as $18-$20 for just the carbohydrate fractions. Others are up to $60-$90 and include all the minerals.
“For the average small horse farm owner who gets hay every week or so, testing might not be feasible, and many hay growers or dealers will not have their hay tested,” said Williams. “Be aware that there is no way to estimate soluble carbohydrate fractions of hay. So, if someone tells you they can, I would be skeptical and get proof by analyzing it!”
Soaking Hay
If an owner is concerned about sugars and starches in forage, it would be smart to soak the hay. Soaking for even just 30 minutes in cold water can remove about 30% of the soluble carbohydrates, including sugar and starch, said Williams.
“Soaking hay would be wise for horses at boarding barns where the hay is too variable to test,” she noted. “It does not need to soak for very long. Using a muck tub or wheelbarrow is an easy way to soak an entire hay net.”
Frank added, “Management strategies are effective in most cases, but some horses require medical treatments prescribed by veterinarians. For example, you can administer levothyroxine to induce weight loss. New drugs called sodium-glucose cotransporter 2 (SGLT2) inhibitors lower blood insulin concentrations.”

Felled by Founder
The most important clinical consequence of insulin dysregulation is hyperinsulinemia-associated laminitis (HAL), which is the most common form of laminitis. It is more common than inflammatory-induced (e.g., following placentitis, colitis), carbohydrate overload or supporting limb laminitis.
“Prolonged hyperinsulinemia induces laminitis. This form of laminitis has different pathologic features to that of an inflammatory-induced laminitis,” explained Professor Martin Sillence, PhD, academic program director (Science)
at Queensland University of Technology. Sillence has academic degrees in Pharmacology, Further Education, and Animal Physiology and Nutrition.
He said, “Changes in the foot are initially observed in the secondary epidermal lamella (SEL). They are characterized by lengthening, narrowing and tapering of those SELs. However, the precise mechanisms responsible for HAL remain unclear.”
Suggested theories include glucose toxicity, matrix metalloproteinase up-regulation or over-stimulation of insulin-like growth factor receptors causing increased cell proliferation.
HAL Research
Vets and owners should not take HAL lightly. One study showed that one-third of horses diagnosed with HAL are euthanized within the first year of being diagnosed. It will recur in approximately one-third of “recovered” horses (de Laat et al., 2019).
Once horses become laminitic, key questions owners might ask are: 1) What are the chances of the horse recovering? and 2) How long will the recovery process take?
Sillence and his team at Queensland University of Technology have worked closely with Boehringer Ingelheim Vetmedica and a team of equine clinicians in Germany to answer these questions. Sillence and colleagues analyzed data collected from 37 horses diagnosed with naturally occurring HAL from 16 equine clinics located in Germany. They assessed laminitis severity in each of those horses on Day 0 (the day they entered the trial) and again on Days 4,
9, 14, 25 and 42.
For the first nine days of the study, horses were confined to stalls/rested and restricted to hay-only diets. Some wore supportive pads and bandages.
After the first nine days, management—including diet—was as prescribed by the individual veterinarian managing the case. Researchers allowed included horses non-steroidal anti-inflammatory drugs but not levothyroxine, metformin or corticosteroids.
EMS Research Results
Of the included 37 equids, 19 (51%) were horses, the median age was 17 years, and 81% were fat or very fat. Further, 57% had a history of laminitis. “When the individual clinical laminitis scores were plotted against time, almost three-quarters of the horses improved rapidly, within two weeks of the onset of laminitis,” said Sillence. “Those horses had a median laminitis lameness score of 0 by Day 14.
“The remaining equids—about one in four—improved much slower, with a laminitis lameness score of 5 out of 12 by Day 14,” he added.
Three key variables associated with a more rapid rate of improvement were age, blood glucose and insulin levels.
Younger horses were more likely to recover slowly. And while circulating insulin and glucose levels were within the normal range in all horses after transitioning to the hay-only diet in the first nine days, levels of insulin and glucose were still slightly higher in the slow responders than the fast responders.
Key Research Takeaways
“An important message here is that we found a link between insulin, glucose and slower recovery. This is consistent with insulin being the causative agent of HAL,” noted Sillence. “We have a good idea of the insulin threshold for triggering moderately severe HAL from earlier studies in ponies. Beyond that threshold, we showed that the risk of laminitis increased in proportion to their insulin concentration. But the study on laminitis recovery has led us to understand that more work is needed before we can know how much insulin is needed to cause moderate damage to the hoof or impair recovery.”
Another interesting aspect of the study was that it used a 12-point lameness scale in addition to the traditional five-point Obel scale. Sillence and colleagues found that the Obel was not detailed enough to be able to detect subtle changes in lameness. (See the article by Meier et al. 2021 for additional information on the 12-point lameness scale proposed for HAL.)
When horses develop HAL, veterinarians can re-evaluate lameness after about four days. Horses that recover well should show some improvement by then.
“If there is no improvement after four days, then revisit the diet,” said Sillence.
Take-Home Message
Equine metabolic disease and insulin dysregulation occur commonly and have important clinical consequences, particularly HAL. As many owners are unfamiliar with equine metabolic syndrome, veterinarians need to actively educate owners regarding this condition to facilitate early diagnosis and intervention.
Sillence said, “HAL is hard to manage but is preventable with appropriate diet and/or medications, such as insulin-lowering agents, even in some of the most difficult cases. We are actively researching preventative and treatment strategies.”